Vascular & Varicose Veins
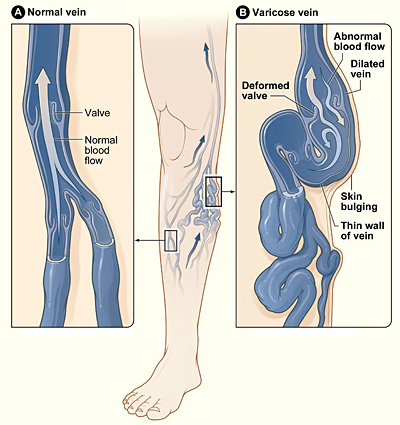
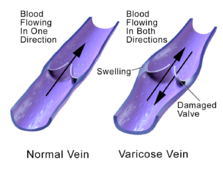
Varicose veins are veins that have become enlarged and tortuous (twisted). The term commonly refers to the veins on the leg, although varicose veins can occur elsewhere. Veins have leaflet valves to prevent blood from flowing backwards (retrograde flow or reflux). Leg muscles pump the veins to return blood to the heart (the skeletal-muscle pump), against the effects of gravity. When veins become varicose, the leaflets of the valves no longer meet properly, and the valves do not work (valvular incompetence). This allows blood to flow backwards and they enlarge even more.
Varicose veins are most common in the superficial veins of the legs, which are subject to high pressure when standing. Besides being a cosmetic problem, varicose veins can be painful, especially when standing. Severe long-standing varicose veins can lead to leg swelling, venous eczema, skin thickening (lipodermatosclerosis) and ulceration. Life-threatening complications are uncommon, but varicose veins may be confused with deep vein thrombosis, which may be life-threatening.
Non-surgical treatments include elastic stockings, elevating the legs, and exercise. Surgical treatment involves vein stripping to remove the affected veins. Because most of the blood in the legs is returned by the deep veins, the superficial veins, which return only about 10% of the total blood of the legs, can usually be removed without serious harm.
Secondary varicose veins are those developing as collateral pathways, typically after stenosis or occlusion of the deep veins, a common sequel of extensive deep vein thrombosis (DVT). Varicose veins are distinguished from reticular veins (blue veins) and telangiectasias (spider veins), which also involve valvular insufficiency, by the size and location of the veins.
- Aching, heavy legs (often worse at night and after exercise).
- Appearance of spider veins (telangiectasia) in the affected leg.
- Ankle swelling, especially in evening.
- A brownish-yellow shiny skin discoloration near the affected veins.
- Redness, dryness, and itchiness of areas of skin, termed stasis dermatitis or venous eczema, because of waste products building up in the leg.
- Cramps may develop especially when making a sudden move as standing up.
- Minor injuries to the area may bleed more than normal or take a long time to heal.
- In some people the skin above the ankle may shrink (lipodermatosclerosis) because the fat underneath the skin becomes hard.
- Restless legs syndrome appears to be a common overlapping clinical syndrome in patients with varicose veins and other chronic venous insufficiency.
- Whitened, irregular scar-like patches can appear at the ankles. This is known as atrophie blanche.
Traditionally, varicose veins were only investigated using imaging techniques if there was a clinical suspicion of deep venous insufficiency, if they were recurrent, or if they involved the sapheno-popliteal junction. This practice is not now widely accepted. All patients with varicose veins should now be investigated using Duplex Doppler ultrasound scanning. The results from a randomised controlled trial (RCT) on the follow-up of patients with and without routine Duplex scan has shown a significant difference in recurrence rate and reoperation rate at 2 and 7 years of follow-up.
Most varicose veins are reasonably benign, but severe varicosities can lead to major complications, due to the poor circulation through the affected limb.
- Pain, tenderness, heaviness, inability to walk or stand for long hours, thus hindering work
- Skin conditions / Dermatitis which could predispose skin loss
- Skin ulcers especially near the ankle, usually referred to as venous ulcers.
- Development of carcinoma or sarcoma in longstanding venous ulcers. There have been over 100 reported cases of malignant transformation and the rate is reported as 0.4% to 1%.
- Severe bleeding from minor trauma, of particular concern in the elderly.
- Blood clotting within affected veins. Termed superficial thrombophlebitis. These are frequently isolated to the superficial veins, but can extend into deep veins becoming a more serious problem.
- Acute fat necrosis can occur, especially at the ankle of overweight patients with varicose veins. Females are more frequently affected than males.
Varicose veins are more common in women than in men, and are linked with heredity. Other related factors are pregnancy, obesity, menopause, aging, prolonged standing, leg injury, and abdominal straining. Varicose veins are unlikely to be caused by crossing the legs or ankles. Less commonly, but not exceptionally, varicose veins can be due to other causes, as post phlebitic obstruction or incontinence, venous and arteriovenous malformations.
Varicose veins could also be caused by elevated levels of homocysteine in the body, which can degrade and inhibit the formation of the three main structural components of the artery: collagen, elastin and the proteoglycans. Homocysteine permanently degrades cysteine disulfide bridges and lysine amino acid residues in proteins, gradually affecting function and structure. Simply put, homocysteine is a ‘corrosive’ of long-living proteins, i.e. collagen or elastin, or lifelong proteins, i.e. fibrillin. These long-term effects are difficult to establish in clinical trials focusing on groups with existing artery decline.
Conservative
The symptoms of varicose veins can be controlled to an extent with the following:
- Elevating the legs often provides temporary symptomatic relief.
- Regular exercise.
- The wearing of graduated compression stockings with variable pressure gradients (Class II or III) has been shown to correct the swelling, nutritional exchange, and improve the microcirculation in legs affected by varicose veins. They also often provide relief from the discomfort associated with this disease. Caution should be exercised in their use in patients with concurrent arterial disease.
- The wearing of intermittent pneumatic compression devices have been shown to reduce swelling and increase circulation.
- Anti-inflammatory medication such as ibuprofen or aspirin can be used as part of treatment for superficial thrombophlebitis along with graduated compression hosiery – but there is a risk of intestinal bleeding. In extensive superficial thrombophlebitis, consideration should be given to anti-coagulation and thrombectomy of the involved vein.
- Topical gel application, helps in managing symptoms related to varicose veins such as inflammation, pain, swelling, itching and dryness.
Surgical
Several techniques have been performed for over a century, from the more invasive saphenous stripping, to less invasive procedures like stab avulsions.
- Stripping. Stripping consists of removal of all or part the saphenous vein (great/long or lesser/short) main trunk. The complications include deep vein thrombosis (5.3%), pulmonary embolism (0.06%), and wound complications including infection (2.2%). Reported recurrence rates, which have been tracked for 10 years, are about 5–10%.
- Stab avulsions
- Vein ligation
- Infusaport / Portacath
- Amputation




