Gallbladder & Liver
Gallstones
A gallstone is a lump of hard material usually range in size from a grain of sand to 3-4cms. They are formed inside the gall bladder formed as a result of precipitation of cholesterol and bile salts from the bile.
- Cholesterol stones
- Pigment stones
- Mixed stones – the most common type. They are comprised of cholesterol and salts
Cholesterol stones are usually yellow-green and are made primarily of hardened cholesterol. They account for about 80 percent of gallstones. Scientists believe cholesterol stones form when bile contains too much cholesterol, too much bilirubin, or not enough bile salts, or when the gallbladder does not empty as it should for some other reason.
Pigment stones are small, dark stones made of bilirubin. The exact cause is not known. They tend to develop in people who have cirrhosis, biliary tract infections, and hereditary blood disorders such as sickle cell anaemia in which too much bilirubin is formed. Other causes are related to excess excretion of cholesterol by liver through bile.
They include the following:
- Gender – Women between 20 and 60 years of age are twice as likely to develop gallstones as men
- Obesity – Obesity is a major risk factor for gallstones, especially in women
- Oestrogen – Excess oestrogen from pregnancy, hormone replacement therapy, or birth control pills
- Cholesterol-lowering drugs
- Diabetes – People with diabetes generally have high levels of fatty acids called triglycerides
- Rapid weight loss – As the body metabolizes fat during rapid weight loss, it causes the liver to secrete extra cholesterol into bile, which can cause gallstones
- Indigestion & belching
Many people with gallstones have no symptoms. These patients are said to be asymptomatic, and these stones are called “silent stones.” Gallstone symptoms are similar to those of heart attack, appendicitis, ulcers, irritable bowel syndrome, hiatal hernia, pancreatitis, and hepatitis. So accurate diagnosis is important.
Symptoms may vary and often follow fatty meals, and they may occur during the night.
- Abdominal bloating
- Recurring intolerance of fatty foods
- Steady pain in the upper abdomen that increases rapidly and lasts from 30 minutes to several hours
- Pain in the back between the shoulderblades
- Pain under the right shoulder
- Nausea or vomiting
- Indigestion & belching
Ultrasound is the most sensitive and specific test for gallstones. Other diagnostic tests may include:
- Computed tomography (CT) scan may show the gallstones or complications
- Endoscopic retrograde cholangiopancreatography (ERCP). The patient swallows an endoscope–a long, flexible, lighted tube connected to a computer and TV monitor. The doctor guides the endoscope through the stomach and into the small intestine.
- The doctor then injects a special dye that temporarily stains the ducts in the biliary system. ERCP is used to locate and remove stones in the ducts
- Blood tests. Blood tests may be used to look for signs of infection, obstruction, pancreatitis, or jaundice
Bile-duct blockage and infection caused by stones in the biliary tract can be a life-threatening illness. With prompt diagnosis and treatment, the outcome is usually very good.
The obstruction caused by gall stone may lead to Biliary colic, Inflammation of gall bladder (Cholecystitis). Other complications may include:
- Cirrhosis – Cirrhosis is the result of chronic liver disease that causes scarring of the liver (fibrosis – nodular regeneration) and liver dysfunction
- Cholangitis – Cholangitis is an infection of the common bile duct, which carries bile (which helps in digestion) from the liver to the gallbladder and then to the intestines
Surgery
Surgery to remove the gallbladder is the most common way to treat symptomatic gallstones. The most common operation is called laparoscopic cholecystectomy. For this operation, the surgeon makes several tiny incisions in the abdomen and inserts surgical instruments and a miniature video camera into the abdomen. The camera sends a magnified image from inside the body to a video monitor, giving the surgeon a close up view of the organs and tissues. While watching the monitor, the surgeon uses the instruments to carefully separate the gallbladder from the liver, ducts, and other structures.
If gallstones are in the bile ducts, the physician (usually a gastroenterologist) may use endoscopic retrograde cholangiopancreatography (ERCP) to locate and remove them before or during the gallbladder surgery.
Laparoscopic Cholecystectomy
Gallbladder removal is one of the most commonly performed surgical procedures in Australia. Today, gallbladder surgery is performed laparoscopically. The medical name for this procedure is Laparoscopic Cholecystectomy.
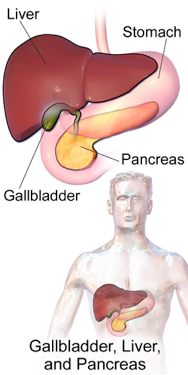
- The gallbladder is a pear-shaped organ that rests beneath the right side of the liver.
- Its main purpose is to collect and concentrate a digestive liquid (bile) produced by the liver. Bile is released from the gallbladder after eating, aiding digestion. Bile travels through narrow tubular channels (bile ducts) into the small intestine.
- Removal of the gallbladder is not associated with any impairment of digestion in most people.
- Gallbladder problems are usually caused by the presence of gallstones: small hard masses consisting primarily of cholesterol and bile salts that form in the gallbladder or in the bile duct.
- It is uncertain why some people form gallstones.
- There is no known means to prevent gallstones.
- These stones may block the flow of bile out of the gallbladder, causing it to swell and resulting in sharp abdominal pain, vomiting, indigestion and, occasionally, fever.
- If the gallstone blocks the common bile duct, jaundice (a yellowing of the skin) can occur.
Ultrasound is most commonly used to find gallstones.
In a few more complex cases, other X-ray tests may be used to evaluate gallbladder disease.
Gallstones do not go away on their own. Some can be temporarily managed with drugs or by making dietary adjustments, such as reducing fat intake. This treatment has a low, short-term success rate. Symptoms will eventually continue unless the gallbladder is removed.Surgical removal of the gallbladder is the time honoured and safest treatment of gallbladder disease.
- Rather than a five to seven inch incision, the operation requires only four small openings in the abdomen.
- Patients usually have minimal post-operative pain.
- Patients usually experience faster recovery than open gallbladder surgery patients.
- Most patients go home within one day and enjoy a quicker return to normal activities.
Although there are many advantages to laparoscopy, the procedure may not be appropriate for some patients who have had previous upper abdominal surgery or who have some pre-existing medical conditions. A thorough medical evaluation by your personal physician, in consultation with a surgeon trained in laparoscopy, can determine if laparoscopic gallbladder removal is an appropriate procedure for you.
The following includes typical events that may occur prior to laparoscopic surgery; however, since each patient and surgeon is unique, what will actually occur may be different:
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an ECG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Your surgeon may request that you completely empty your colon and cleanse your intestines prior to surgery. You may be requested to drink clear liquids, only, for one or several days prior to surgery.
- It is recommended that you shower the night before or morning of the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
- Under general anaesthesia, so the patient is asleep throughout the procedure.
- Using a cannula (a narrow tube-like instrument), the surgeon enters the abdomen in the area of the belly-button.
- A laparoscope (a tiny telescope) connected to a special camera is inserted through the cannula, giving the surgeon a magnified view of the patient’s internal organs on a television screen.
- Other cannulas are inserted which allow your surgeon to delicately separate the gallbladder from its attachments and then remove it through one of the openings.
- Many surgeons perform an X-ray, called a cholangiogram, to identify stones, which may be located in the bile channels, or to insure that structures have been identified.
- If the surgeon finds one or more stones in the common bile duct, (s)he may remove them with a special scope, may choose to have them removed later through a second minimally invasive procedure, or may convert to an open operation in order to remove all the stones during the operation.
- After the surgeon removes the gallbladder, the small incisions are closed with a stitch or two or with surgical tape.
In a small number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.




