Hand & Foot
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a condition brought on by increased pressure on the median nerve at the wrist. In effect, it is a pinched nerve at the wrist. Symptoms may include numbness, tingling, and pain in the arm, hand, and fingers. There is a space in the wrist called the carpal tunnel where the median nerve and nine tendons pass from the forearm into the hand (see Figure 1). Carpal tunnel syndrome happens when pressure builds up from swelling in this tunnel and puts pressure on the nerve. When the pressure from the swelling becomes great enough to disturb the way the nerve works, numbness, tingling, and pain may be felt in the hand and fingers (see Figure 2).

Usually the cause is unknown. Pressure on the nerve can happen several ways: swelling of the lining of the flexor tendons, called tenosynovitis; joint dislocations, fractures, and arthritis can narrow the tunnel; and keeping the wrist bent for long periods of time. Fluid retention during pregnancy can cause swelling in the tunnel and symptoms of carpal tunnel syndrome, which often go away after delivery. Thyroid conditions, rheumatoid arthritis, and diabetes also can be associated with carpal tunnel syndrome. There may be a combination of causes.
Carpal tunnel syndrome symptoms usually include pain, numbness, tingling, or a combination of the three. The numbness or tingling most often takes place in the thumb, index, middle, and ring fingers. The symptoms usually are felt during the night but also may be noticed during daily activities such as driving or reading a newspaper. Patients may sometimes notice a weaker grip, occasional clumsiness, and a tendency to drop things. In severe cases, sensation may be permanently lost and the muscles at the base of the thumb slowly shrink (thenaratrophy), causing difficulty with pinch.
A detailed history including medical conditions, how the hands have been used, and whether there were any prior injuries is important. An x-ray may be taken to check for the other causes of the complaints such as arthritis or a fracture. In some cases, laboratory tests may be done if there is a suspected medical condition that is associated with CTS. A nerve conduction study (NCV) and/or electromyogram (EMG) may be done to confirm the diagnosis of carpal tunnel syndrome as well as to check for other possible nerve problems.
Symptoms may often be relieved without surgery. Identifying and treating medical conditions, changing the patterns of hand use, or keeping the wrist splinted in a straight position may help reduce pressure on the nerve. Wearing wrist splints at night may relieve the symptoms that interfere with sleep. A steroid injection into the carpal tunnel may help relieve the symptoms by reducing swelling around the nerve.
When symptoms are severe or do not improve, surgery may be needed to make more room for the nerve. Pressure on the nerve is decreased by cutting the ligament that forms the roof (top) of the tunnel on the palm side of the hand (see Figure 3). Incisions for this surgery may vary, but the goal is the same: to enlarge the tunnel and decrease pressure on the nerve. Following surgery, soreness around the incision may last for several weeks or months. The numbness and tingling may disappear quickly or slowly. It may take several months for strength in the hand and wrist to return to normal. Carpal tunnel symptoms may not completely go away after surgery, especially in severe cases.
Carpal Tunnel Release
Carpal tunnel syndrome (CTS) is a condition that causes tingling, pain, numbness, and other symptoms in the distribution of the median nerve due to its compression at the wrist in the carpal tunnel. It appears to be caused by a combination of genetic and environmental factors. Some of the predisposing factors include: diabetes, obesity, pregnancy, hypothyroidism, and heavy manual work or work with vibrating tools. There is some evidence that lighter, repetitive tasks can cause carpal tunnel syndrome.
The main symptom of CTS is intermittent numbness of the thumb, index, long and half of the ring finger. The numbness often occurs at night, with the hypothesis that the wrists are held flexed during sleep. Recent literature suggests that sleep positioning, such as sleeping on one’s side, might be an associated factor. It can be relieved by wearing a wrist splint that prevents flexion. Long-standing CTS leads to permanent nerve damage with constant numbness, wasting of some of the muscles of the thumb, and weakness.
Pain in carpal tunnel syndrome is primarily numbness that is so intense that it wakes one from sleep. Pain in electrophysiologically verified CTS is associated with misinterpretation of nociception and depression.
Conservative treatments include use of night splints and corticosteroid injection. The only scientifically established disease modifying treatment is surgery to cut the transverse carpal ligament
People with CTS experience numbness, tingling, or burning sensations in the thumb and fingers, in particular the index, middle fingers, and half of the ring fingers, which are innervated by the median nerve. Less-specific symptoms may include pain in the wrists or hands and loss of grip strength (both of which are more characteristic of painful conditions such as arthritis).
Some suggest that median nerve symptoms can arise from compression at the level of the neck or in the forearm, but this is debatable. This line of thinking is an attempt to explain pain and other symptoms not characteristic of carpal tunnel syndrome.
Numbness and paresthesias in the median nerve distribution are the hallmark symptoms of carpal tunnel entrapment syndrome. Weakness and wasting of the thumb muscles may occur if the condition remains untreated.

Generally accepted treatments include: steroids either orally or injected locally, splinting, and surgical release of the transverse carpal ligament. There is no or insufficient evidence for ultrasound, yoga, lasers, B6, and exercise therapy. Early surgery with carpal tunnel release is indicated where there is clinical evidence of median nerve denervation or a person elects to proceed directly to surgical treatment.
The importance of wrist braces and splints in the carpal tunnel syndrome therapy is known, but many people are unwilling to use braces. Current recommendations generally don’t suggest immobilizing braces, but instead activity modification and non-steroidal anti-inflammatory drugs as initial therapy, followed by more aggressive options or specialist referral if symptoms do not improve.
Many health professionals suggest that, for the best results, one should wear braces at night and, if possible, during the activity primarily causing stress on the wrists.

Corticosteroid injections can be effective for temporary relief from symptoms while a person develops a long-term strategy that fits their lifestyle. This treatment is not appropriate for extended periods, however. In general, local steroid injections are only used until other treatment options can be identified. For most surgery is the only option that will provide permanent relief.
Carpal tunnel surgery, also called carpal tunnel release and carpal tunnel decompression surgery, is a surgery in which the transverse carpal ligament is released. It is a treatment for carpal tunnel syndrome and recommended when there is troublesome numbness, muscle weakness or symptoms of pain in the carpal tunnel. In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment.
Surgery involves an incision on the palm about an 2-3cm in length. Through this incision, the skin and subcutaneous tissue is divided, followed by the palmar fascia, and ultimately the transverse carpal ligament.
Trigger Finger
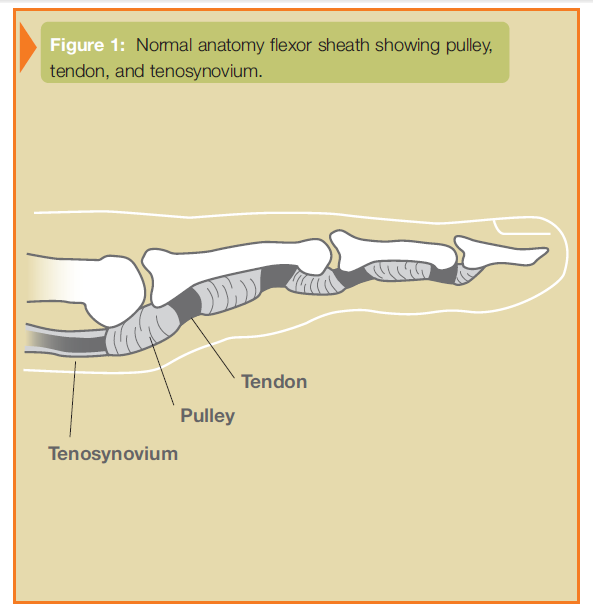
Stenosing tenosynovitis, commonly known as “trigger finger” or “trigger thumb”, involves the pulleys and tendons in the hand that bend the fingers. The tendons work like long ropes connecting the muscles of the forearm with the bones of the fingers and thumb. In the finger, the pulleys are a series of rings that form a tunnel through which the tendons must glide, much like the guides on a fishing rod through which the line (or tendon) must pass. These pulleys hold the tendons close against the bone. The
tendons and the tunnel have a slick lining that allows easy gliding of the tendon through the pulleys (see Figure 1).
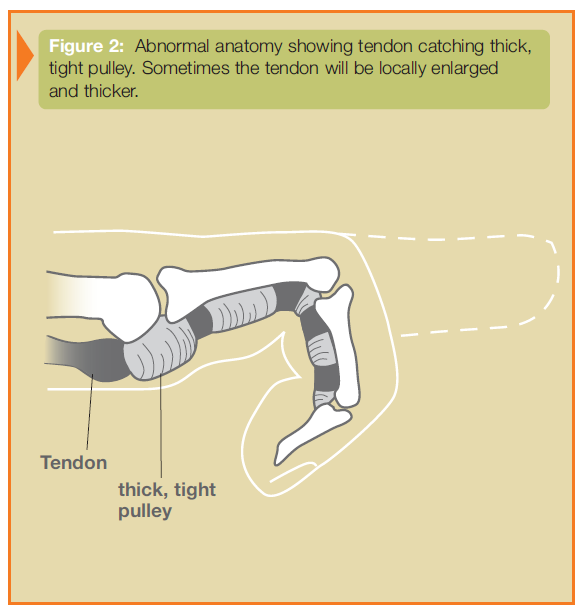
Trigger finger/thumb occurs when the pulley at the base of the finger becomes too thick and constricting around the tendon, making it hard for the tendon to move freely through the pulley. Sometimes the tendon develops a nodule (knot) or swelling of its lining. Because of the increased resistance to the gliding of the tendon through the pulley, one may feel pain, popping, or a catching feeling in the finger or thumb (see Figure 2). When the tendon catches, it produces inflammation and more swelling. This causes a vicious cycle of triggering, inflammation, and swelling. Sometimes the finger becomes stuck or locked, and is hard to straighten or bend.
Causes for this condition are not always clear. Some trigger fingers are associated with medical conditions such as rheumatoid arthritis, gout, and diabetes. Local trauma to the palm/base of the finger may be a factor on occasion, but in most cases there is not a clear cause.
Trigger finger/thumb may start with discomfort felt at the base of the finger or thumb, where they join the palm. This area is often tender to local pressure. A nodule may sometimes be found in this area. When the finger begins to trigger or lock, the patient may think the problem is at the middle knuckle of the finger or the tip knuckle of the thumb, since the tendon that is sticking is the one that moves these joints.
The goal of treatment in trigger finger/thumb is to eliminate the catching or locking and allow full movement of the finger or thumb without discomfort. Swelling around the flexor tendon and tendon sheath must be reduced to allow smooth gliding of the tendon. The wearing of a splint or taking an oral anti-inflammatory medication may sometimes help. Treatment may also include changing activities to reduce swelling. An injection of steroid into the area around the tendon and pulley is often effective in relieving the trigger finger/thumb.
If non-surgical forms of treatment do not relieve the symptoms, surgery may be recommended. This surgery is performed as an outpatient, usually with simple local anesthesia. The goal of surgery is to open the pulley at the base of the finger so that the tendon can glide more freely. Active motion of the finger generally begins immediately after surgery. Normal use of the hand can usually be resumed once comfort permits. Some patients may feel tenderness, discomfort, and swelling about the area of their surgery longer than others. Occasionally, hand therapy is required after surgery to regain better use.
Ganglion Cysts
Ganglion cysts are very common lumps within the hand and wrist that occur adjacent to joints or tendons. The most common locations are the top of the wrist (see Figure 1), the palm side of the wrist, the base of the finger on the palm side, and the top of the end joint of the finger. The ganglion cyst often resembles a water balloon on a stalk (see Figure 2), and is filled with clear fluid or gel. The cause of these cysts is unknown although they may form in the presence of joint or tendon irritation or mechanical changes. These cysts may change in size or even disappear completely, and they may or may not be painful. These cysts are not cancerous and will not spread to other areas.

The diagnosis is usually based on the location of the lump and its clinical appearance. They are usually oval or round and may be soft or very firm. Cysts at the base of the finger on the palm side are typically a very firm, pea-sized nodule that is tender to applied pressure, such as when gripping. Light will often pass through these lumps (trans-illumination) and this can assist in the diagnosis. Your physician may request x-rays in order to investigate problems in adjacent joints; cysts at the end joint of the finger frequently have an arthritic bone spur associated with them.
Treatment can often be non-surgical. In many cases, these cysts can simply be observed, especially if they are painless. If the cyst becomes painful, limits activity, or is cosmetically unacceptable, other treatment options are available. The use of splints and anti-inflammatory medication can be prescribed in order to decrease pain associated with activities. An aspiration can be performed to remove the fluid from the cyst and decompress it. This requires placing a needle into the cyst, which can be performed in most office settings. If non-surgical options fail to provide relief or if the cyst recurs, surgical alternatives are available. Surgery involves removing the cyst along with a portion of the joint capsule or tendon sheath (see Figure 3). In the case of wrist ganglion cysts, both traditional open and arthroscopic techniques may yield good results. Surgical treatment is generally successful although cysts may recur. Your surgeon will discuss the best treatment options for you.

Dupuytren’s Disease
Dupuytren’s disease is an abnormal thickening of the fascia (the tissue just beneath the skin of the palm). It often starts with firm lumps in the palm. In some patients, firm cords will develop beneath the skin, stretching from the palm into the fingers (see Figure 1). Gradually, these cords may cause the fingers to bend into the palm (see Figure 2). Although the skin may become involved in the process, the deeper structures—such as the tendons—are not directly involved. Occasionally, the disease will cause thickening on top of the finger knuckles (knuckle pads), or nodules or cords within the soles of the feet (plantar fibromatosis).

The cause of Dupuytren’s disease is unknown but may be associated with certain biochemical factors within the involved fascia. The problem is more common in men over age 40 and in people of northern European descent. There is no proven evidence that hand injuries or specific occupational exposures lead to a higher risk of developing Dupuytren’s disease.
Symptoms of Dupuytren’s disease usually include a small lump or series of lumps and pits within the palm. The lumps are generally firm and adherent to the skin. Gradually a cord may develop, extending from the palm into one or more fingers, with the ring and little fingers most commonly affected. These cords may be mistaken for tendons, but they actually lie between the skin and the tendons. In many cases, both hands are affected, although the degree of involvement may vary.
The initial nodules may produce discomfort that usually resolves, but Dupuytren’s disease is not typically painful. The disease may first be noticed because of difficulty placing the hand flat on an even surface, such as a tabletop (see Figure 3). As the fingers are drawn into the palm, one may notice increasing difficulty with activities such as washing, wearing gloves, shaking hands, and putting hands into pockets. Progression is unpredictable. Some individuals will have only small lumps or cords while others will develop severely bent fingers. More severe disease often occurs with an earlier age of onset.
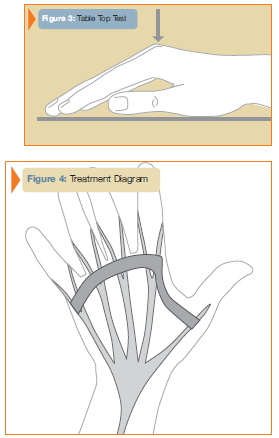
In some cases, only observation is needed for nodules and cords that are not contracted. Patients with more advanced contractures may require surgery in order to improve function. Various surgical techniques are available in order to correct finger position. Your treating surgeon will discuss the method most appropriate for your condition based upon the stage of the disease and the joints involved (see Figure 4). The goal of surgery is to improve finger position and thereby hand function. Despite surgery, the disease process may recur and the fingers may begin to bend into the palm once again. Before surgery, your treating surgeon
will discuss realistic goals and results.
Specific surgical considerations:
- The presence of a lump in the palm does not mean that surgery is required or that the
disease will progress. - Correction of finger position is best accomplished with milder contractures and
contractures that affect the base of the finger. Complete correction sometimes can not
be attained, especially of the middle and end joints in the finger. - Skin grafts are sometimes required to cover open areas in the fingers if the skin is
deficient. - The nerves that provide feeling to the fingertips are often intertwined with the cords.
- Splinting and hand therapy are often required after surgery in order to maximize and
maintain the improvement in finger position and function.




