Hernia Repair
A hernia is a weakness or defect in the abdominal wall. It may be present from birth, or develop over a period of time. If the defect is large enough, abdominal contents such as the bowels, may protrude through the defect causing a lump or bulge felt by the patient.
Hernias develop at certain sites which have a natural tendency to be weak; the groin, umbilicus (belly button), and previous surgical incisions.
- Lump in groin area when standing/straining & disappears when reclining
- Pain at the site of the lump, especially when lifting a heavy object
- Swelling of the scrotum
- Excruciating abdominal pain (if you have strangulation)
- Nausea, vomiting, loss of appetite & pain (if intestinal obstruction occurs)
Once a hernia has developed, it will tend to enlarge and cause discomfort. If a loop of bowel gets caught in the hernia, it may become obstructed or its blood supply may be cut off. This could then become a life-threatening situation. Since hernias can be repaired effectively and with minimal risk, most surgeons therefore recommend that hernias be repaired when diagnosed, unless there is serious medical problem which makes it too risky.
Hernia Repair (Surgery)
The standard method of hernia repair involves making an incision in the abdominal wall. Normal healthy tissues are cut until the area of weakness is found. This area, the hernia, is then repaired with sutures. Often a prosthetic material, or another plastic material, is sutured in place to strengthen the area of weakness. Finally, the skin and other healthy tissues that were cut at the beginning are sutured back together to complete the repair.
Newer hernia repair involves minimally invasive laparoscopic techniques. However, hernia operation with open techniques is still a valid option reaching the highest standards of care. Laparoscopic techniques of hernia repair are especially attractive when patients are dealing with recurrent hernias or bilateral inguinal hernias.
Inguinal Hernia Repair
- A hernia occurs when the inside layers of the abdominal muscle have weakened, resulting in a bulge or tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a small balloon-like sac. This can allow a loop of intestine or abdominal tissue to push into the sac. The hernia can cause severe pain and other potentially serious problems that could require emergency surgery.
- Both men and women can get a hernia.
- You may be born with a hernia (congenital) or develop one over time.
- A hernia does not get better over time, nor will it go away by itself.
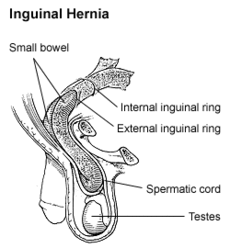

- The common areas where hernias occur are in the groin (inguinal), belly button (umbilical), and the site of a previous operation (incisional).
- It is usually easy to recognize a hernia. You may notice a bulge under the skin. You may feel pain when you lift heavy objects, cough, strain during urination or bowel movements, or during prolonged standing or sitting.
- The pain may be sharp and immediate or a dull ache that gets worse toward the end of the day.
- Severe, continuous pain, redness, and tenderness are signs that the hernia may be entrapped or strangulated. These symptoms are cause for concern and immediate contact of your physician or surgeon.
The wall of the abdomen has natural areas of potential weakness. Hernias can develop at these or other areas due to heavy strain on the abdominal wall, aging, injury, an old incision or a weakness present from birth. Anyone can develop a hernia at any age. Most hernias in children are congenital. In adults, a natural weakness or strain from heavy lifting, persistent coughing, difficulty with bowel movements or urination can cause the abdominal wall to weaken or separate.
Laparoscopic Hernia Repair is a technique to fix tears in the abdominal wall (muscle) using small incisions, telescopes and a patch (mesh). If may offer a quicker return to work and normal activities with decreased pain.
Only after a thorough examination can your surgeon determine whether laparoscopic hernia repair is right for you. The procedure may not be best for some patients who have had previous abdominal surgery or underlying medical conditions.
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an ECG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- It is recommended that you shower the night before or morning of the operation.
- If you have difficulties moving your bowels, an enema or similar preparation may be used after consulting with your surgeon.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
There are few options available for a patient who has a hernia:
- Use of a truss (hernia belt) is rarely prescribed as it is usually ineffective.
- Most hernias require a surgical procedure.
- Surgical procedures are done in one of two fashions.
- The open approach is done from the outside through a three to four inch incision in the groin or the area of the hernia. The incision will extend through the skin, subcutaneous fat, and allow the surgeon to get to the level of the defect. The surgeon may choose to use a small piece of surgical mesh to repair the defect or hole. This technique is usually done with a local anaesthetic and sedation but may be performed using a spinal or general anaesthetic.
- The laparoscopic hernia repair. In this approach, a laparoscope (a tiny telescope) connected to a special camera is inserted through a cannula, a small hollow tube, allowing the surgeon to view the hernia and surrounding tissue on a video screen.
Other cannulas are inserted which allow your surgeon to work “inside.” Three or four quarter inch incisions are usually necessary. The hernia is repaired from behind the abdominal wall. A small piece of surgical mesh is placed over the hernia defect and held in place with small surgical staples. This operation is usually performed with general anaesthesia or occasionally using regional or spinal anaesthesia.
In a small number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.
Abdominal Hernia Repair
Tens of thousands of abdominal hernia repairs are performed each year in Australia. Many are performed by the conventional “open” method. Some are performed laparoscopically (keyhole). If your surgeon has recommended a laparoscopic repair, this information can help you understand what a hernia is and more about the treatment.
Laparoscopic hernia repair is a technique to fix tears or openings in the abdominal wall using small incisions, laparoscopes (small telescopes inserted into the abdomen) and a patch (screen or mesh) to reinforce the abdominal wall. It may offer a quicker return to work and normal activities with decreased pain for some patients.
- When an abdominal hernia occurs, it usually arises in the abdominal wall where a previous surgical incision was made. In this area the abdominal muscles have weakened; this results in a bulge or a tear. In the same way that an inner tube pushes through a damaged tire, the inner lining of the abdomen pushes through the weakened area of the abdominal wall to form a balloon-like sac. This can allow a loop of intestines or other abdominal contents to push into the sac. If the abdominal contents get stuck within the sac, they can become trapped or “incarcerated.” This could lead to potentially serious problems that might require emergency surgery.
- Other sites that abdominal hernias can develop are the belly button (umbilicus) or any other area of the abdominal wall.
- A hernia does not get better over time, nor will it go away by itself.
- A hernia is usually recognized as a bulge under your skin. Occasionally, it causes no discomfort at all, but you may feel pain when you lift heavy objects, cough, strain during urination or bowel movements or with prolonged standing or sitting.
- The discomfort may be sharp or a dull ache that gets worse towards the end of the day. Any continuous or severe discomfort, redness, nausea or vomiting associated with the bulge are signs that the hernia may be entrapped or strangulated. These symptoms are cause for concern and immediate contact of your physician or surgeon is recommended.
- An incision in your abdominal wall will always be an area of potential weakness. Hernias can develop at these sites due to heavy straining, aging, injury or following an infection at that site following surgery. They can occur immediately following surgery or may not become apparent for years later following the procedure.
- Anyone can get a hernia at any age. They are more common as we get older. Certain activities may increase the likelihood of a hernia including persistent coughing, difficulty with bowel movements or urination, or frequent need for straining.
Results may vary depending on the type of procedure and each patient’s overall condition. Common advantages may include:
- Less post-operative pain
- Shortened hospital stay
- Faster return to regular diet
- Quicker return to normal activity
Only after a thorough examination can your surgeon determine whether a laparoscopic abdominal hernia repair is right for you. The procedure may not be best for some patients who have had extensive previous abdominal surgery, hernias found in unusual or difficult to approach locations, or underlying medical conditions. Be sure to consult your physician about your specific case.
- Most hernia operations are performed on an outpatient basis, and therefore the you will probably go home on the same or following day that the operation is performed
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an ECG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- It is recommended that you shower the night before or morning of the operation.
- Your surgeon my request that you completely empty your colon and cleanse your intestines before surgery. Usually, you must drink a special cleansing solution. You may be requested to drink clear liquids, only, for one or several days prior to the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
There are few options available for a patient with an abdominal hernia.
- The use of an abdominal wall binder is occasionally prescribed but often ineffective
- Abdominal hernias do not go away on their own and may enlarge with time.
- Surgery is the preferred treatment and is done in one of two ways:
- The traditional approach is done through an incision in the abdominal wall. It may go through part or all of a previous incision, skin, an underlying fatty layer and into the abdomen. The surgeon may choose to sew your natural tissue back together, but frequently, it requires the placement of mesh (screen) in or on the abdominal wall for a sound closure. This technique is most often performed under a general aesthetic but in certain situations may be done under local anaesthesia with sedation or spinal anaesthesia. Your surgeon will help you select the anaesthesia that is best for you.
- The second approach is a laparoscopic abdominal hernia repair. In this approach, a laparoscope (a tiny telescope with a television camera attached) is inserted through a cannula (a small hollow tube).
The laparoscope and TV camera allow the surgeon to view the hernia from the inside. Other small incisions will be required for other small cannulas for placement of other instruments to remove any scar tissue and to insert a surgical mesh into the abdomen. This mesh, or screen, is fixed under the hernia defect to the strong tissues of the abdominal wall. It is held in place with special surgical tacks and in many instances, sutures. Usually, three or four 1-2cm incisions are necessary. This operation is usually performed under general anaesthesia.
- You usually arrive at the hospital the morning of the operation.
- A qualified medical staff member will typically place a small needle or catheter into your vein to dispense medication during the surgery. Often pre-operative medications, such as antibiotics, may be given.
- Your anaesthesia will last during and up to several hours following surgery.
- Following the operation, you will be taken to the recovery room and remain there until you are fully awake.
- Few patients may go home the same day of surgery, while others may need admission for a day or more post-operatively. The need to stay in the hospital will be determined according to the extent of the operative procedure and your general health.
In a small number of patients the laparoscopic method cannot be performed. Factors that may increase the possibility of choosing or converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, inability to visualize organs or bleeding problems during the operation.
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.




