Anti-Reflux
Reflux
Gastro Oesophageal Reflux Disease (GORD)
The oesophagus carries food from the mouth to the stomach. The lower oesophageal sphincter is a ring of muscle at the bottom of the oesophagus that acts like a valve between the oesophagus and stomach. Gastro-oesophageal reflux disease, or GORD, is a chronic disease that occurs when the lower oesophageal sphincter does not close properly and stomach contents leak back, or reflux, into the oesophagus.
When refluxed stomach acid touches the lining of the oesophagus, it causes a burning sensation in the chest or throat called heartburn. The fluid may even be tasted in the back of the mouth, and this is called acid indigestion. Occasional heartburn is common but does not necessarily mean one has GORD. Heartburn that occurs more than twice a week may be considered GORD, and it can eventually lead to more serious health problems.
Anyone, including infants, children, and pregnant women, can have GORD.
The main symptoms are persistent heartburn and acid regurgitation. Some people have GORD without heartburn. Instead, they experience pain in the chest, hoarseness in the morning, or trouble swallowing. You may feel like you have food stuck in your throat or like you are choking or your throat is tight. GORD can also cause a dry cough and bad breath.
The most frequent symptoms of GORD are so common that they may not be associated with a disease. Self-diagnosis can lead to mistreatment. Consultation with a physician is essential to proper diagnosis and treatment of GORD.
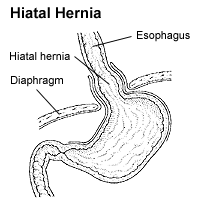
- Hiatal hernia – hiatal hernia occurs when the upper part of the stomach is above the diaphragm, the muscle wall that separates the stomach from the chest.
- Alcohol use
- Overweight
- Pregnancy
- Smoking
Also, certain food and drinks are associated with reflux
- Medical history
- Response to Omeprazole – A recent study 12 demonstrated a potential role for a proton pump inhibitor, omeprazole, in the diagnosis of GORD
- Barium swallow radiograph – Uses x rays to help spot abnormalities such as a hiatal hernia and severe inflammation of the oesophagus
- Endoscopy
Conservative Treatment
- Lifestyle modification
- Medications including antacids, Foaming agents, H2 receptor blockers, Proton Pump inhibitors
Surgical Treatment
Surgery is an option when medicine and lifestyle changes do not work. Surgery may also be a reasonable alternative to a lifetime of drugs and discomfort.
Laparoscopic Nissen Fundoplication
This surgery is performed under general anaesthesia.
If a combination of lifestyle changes and drug therapy does not remedy reflux symptoms, a Nissen Fundoplication can be a very effective surgical procedure to correct reflux. This procedure involves wrapping the upper portion of the stomach around the base of the oesophagus to reinforce the strength of the lower oesophageal sphincter. Until recently, the procedure required a large abdominal incision. A hospital stay of 3-5 days was usually required, and the time to full recovery and return to work was measured in weeks.
A laparoscopic Nissen Fundoplication is a minimally invasive approach that involves specialized video equipment and instruments that allow a surgeon to perform the procedure through four tiny incisions, most of which are less than a half-centimetre in size. One advantage of this method is a brief hospitalization. Most of the time it will require an overnight stay. Other advantages include less pain (less of a need for pain medication), fewer and smaller scars, and a shorter recovery time.
Laparoscopic Nissen Fundoplication is a safe and effective treatment of GORD. However, in rare cases the laparoscopic approach is not possible because it becomes difficult to visualize or handle organs effectively. In such instances, the traditional incision may need to be made to safely complete the operation.
Laparoscopic Anti-Reflux Surgery
Surgery for GORD (“Heartburn”)
If you suffer from “heartburn” your surgeon may have recommended Laparoscopic Anti-Reflux Surgery to treat this condition, technically referred to as gastroesophageal reflux disease (GORD).
Although “heartburn” is often used to describe a variety of digestive problems, in medical terms, it is actually a symptom of gastroesophageal reflux disease (GORD). In this condition, stomach acids reflux or “back up” from the stomach into the oesophagus. Heartburn is described as a harsh, burning sensation in the area in between your ribs or just below your neck. The feeling may radiate through the chest and into the throat and neck. Many adults in Australia experience this uncomfortable, burning sensation at least once a month. Other symptoms may also include vomiting, difficulty swallowing and chronic coughing or wheezing.
When you eat, food travels from your mouth to your stomach through a tube called the oesophagus. At the lower end of the oesophagus is a small ring of muscle called the lower oesophageal sphincter (LOS). The LOS acts like a one-way valve, allowing food to pass through into the stomach. Normally, the LOS closes immediately after swallowing to prevent back-up of stomach juices, which have a high acid content, into the oesophagus. GORD occurs when the LOS does not function properly allowing acid to flow back and burn the lower oesophagus. This irritates and inflames the oesophagus, causing heartburn and eventually may damage the oesophagus.
Some people are born with a naturally weak sphincter (LOS). For others, however, fatty and spicy foods, certain types of medication, tight clothing, smoking, drinking alcohol, vigorous exercise or changes in body position (bending over or lying down) may cause the LOS to relax, causing reflux. A hiatus hernia may be present in many patients who suffer from GORD.
- Lifestyle Changes
In many cases, changing diet and taking over-the-counter antacids can reduce how often and how harsh your symptoms are. Losing weight, reducing or eliminating smoking and alcohol consumption, and altering eating and sleeping patterns can also help. - Drug Therapy
If symptoms persist after these life style changes, drug therapy may be required. Antacids neutralize stomach acids and over-the-counter medications reduce the amount of stomach acid produced. Both may be effective in relieving symptoms. Prescription drugs may be more effective in healing irritation of the oesophagus and relieving symptoms. This therapy needs to be discussed with your surgeon. - Surgery
Patients who do not respond well to lifestyle changes or medications or those who continually require medications to control their symptoms, will have to live with their condition or may undergo a surgical procedure. Surgery is very effective in treating GORD.
There are procedures being tried, known as Intraluminal Endoscopic Procedures, which are alternatives to laparoscopic and open surgery. You will need to discuss with your surgeon and physician whether you are a candidate for any of these procedures.
The advantage of the laparoscopic approach is that it usually provides:
- reduced postoperative pain
- shorter hospital stay
- a faster return to work
- improved cosmetic result
Although laparoscopic anti-reflux surgery has many benefits, it may not be appropriate for some patients. Obtain a thorough medical evaluation by a surgeon qualified in laparoscopic anti-reflux surgery in consultation with your primary care physician or Gastroenterologist to find out if the technique is appropriate for you.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will need to provide written consent for surgery.
- Preoperative preparation includes blood work, medical evaluation, chest x-ray and an ECG depending on your age and medical condition.
- Your surgeon may request that you completely empty your colon and cleanse your intestines prior to surgery. You may be requested to drink clear liquids, only, for one or several days prior to surgery.
- It is recommended that you shower the night before or morning of the operation.
- After midnight the night before the operation, you should not eat or drink anything except medications that your surgeon has told you are permissible to take with a sip of water the morning of surgery.
- Drugs such as aspirin, blood thinners, anti-inflammatory medications (arthritis medications) and Vitamin E will need to be stopped temporarily for several days to a week prior to surgery.
- Diet medication or St. John’s Wort should not be used for the two weeks prior to surgery.
- Quit smoking and arrange for any help you may need at home.
- You usually arrive at the hospital the morning of the operation.
- A qualified medical staff member will place a small needle/catheter in your vein to dispense medication during surgery.
- Often pre-operative medications are necessary.
- You will be under general anaesthesia – asleep – during the operation which may last several hours.
- Following the operation you will be sent to the recovery room until you are fully awake.
- Most patients stay in the hospital the night of surgery and may require additional days in the hospital.
- Laparoscopic anti-reflux surgery (commonly referred to as Laparoscopic Nissen Fundoplication) involves reinforcing the “valve” between the oesophagus and the stomach by wrapping the upper portion of the stomach around the lowest portion of the oesophagus – much the way a bun wraps around a hot dog.
- In a laparoscopic procedure, surgeons use small incisions (1-2cm) to enter the abdomen through cannulas (narrow tube-like instruments). The laparoscope, which is connected to a tiny video camera, is inserted through the small incision, giving the surgeon a magnified view of the patient’s internal organs on a television screen.
- The entire operation is performed “inside” after the abdomen is expanded by inflating gas into it.

In a small number of patients the laparoscopic method is not feasible because of the inability to visualize or handle the organs effectively. Factors that may increase the possibility of converting to the “open” procedure may include obesity, a history of prior abdominal surgery causing dense scar tissue, or bleeding problems during the operation. The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is strictly based on patient safety.





